What is pulmonary stenosis?
 Pulmonary stenosis is a congenital (present at birth) defect that occurs due to abnormal development of the fetal heart during the first eight weeks of pregnancy.
Pulmonary stenosis is a congenital (present at birth) defect that occurs due to abnormal development of the fetal heart during the first eight weeks of pregnancy.
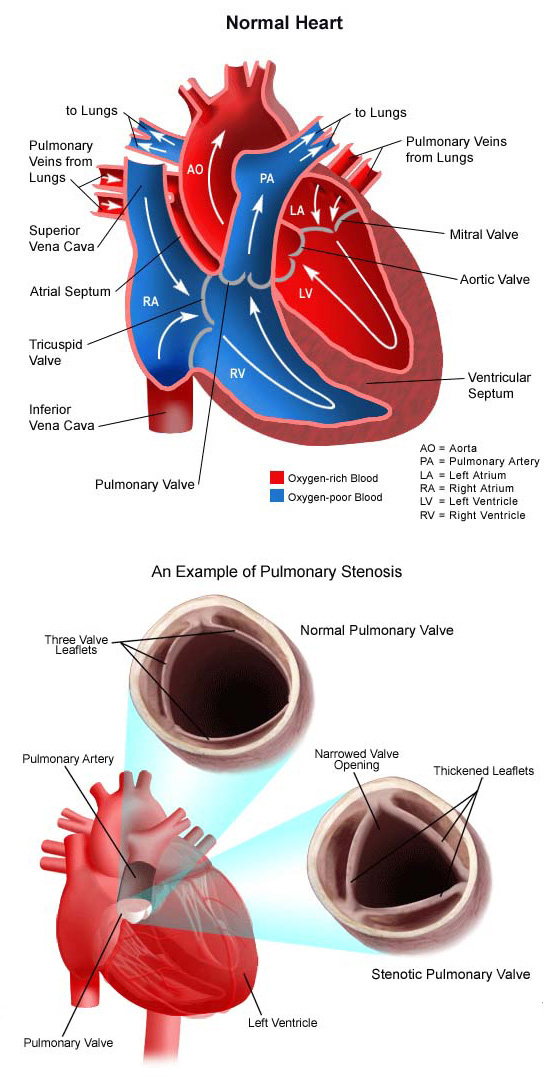
The pulmonary valve is found between the right ventricle and the pulmonary artery. It has three leaflets that function like a one-way door, allowing blood to flow forward into the pulmonary artery, but not backward into the right ventricle.
With pulmonary stenosis, problems with the pulmonary valve make it harder for the leaflets to open and permit blood to flow forward from the right ventricle to the lungs in a normal fashion. In children, these problems can include:
- A valve that has leaflets that are partially fused together.
- A valve that has thick leaflets that do not open all the way.
- The area above or below the pulmonary valve is narrowed.
There are four different types of pulmonary stenosis:
- Valvar pulmonary stenosis. The valve leaflets are thickened and/or narrowed.
- Supravalvar pulmonary stenosis. The pulmonary artery just above the pulmonary valve is narrowed.
- Subvalvar (infundibular) pulmonary stenosis. The muscle under the valve area is thickened, narrowing the outflow tract from the right ventricle.
- Branch peripheral pulmonic stenosis. The right or left pulmonary artery is narrowed, or both may be narrowed.
Pulmonary stenosis may be present in varying degrees, classified according to how much obstruction to blood flow is present. A child with severe pulmonary stenosis could be quite ill, with major symptoms noted early in life. A child with mild pulmonary stenosis may have few or no symptoms, or perhaps none until later in adulthood. A moderate or severe degree of obstruction can become worse with time.
Pulmonary stenosis is a component of half of all complex congenital heart defects.
Pulmonary stenosis accounts for 5 to 10 percent of all congenital heart defect cases.
What causes pulmonary stenosis?
Congenital pulmonary stenosis occurs due to improper development of the pulmonary valve in the first eight weeks of fetal growth. It can be caused by a number of factors, though most of the time this heart defect occurs sporadically (by chance), with no clear reason evident for its development.
Some congenital heart defects may have a genetic link, either occurring due to a defect in a gene, a chromosome abnormality, or environmental exposure, causing heart problems to occur more often in certain families.
Why is pulmonary stenosis a concern?
Mild pulmonary stenosis may not cause any symptoms. Problems can occur when pulmonary stenosis is moderate to severe. When this is the case, the right ventricle has to work harder to try to move blood through the tight pulmonary valve. Eventually, the right ventricle is no longer able to handle the extra workload, and it fails to pump forward efficiently. Pressure builds up in the right atrium, and then in the veins bringing blood back to the right side of the heart. Fluid retention and swelling may occur.
What are the symptoms of pulmonary stenosis?
The following are the most common symptoms of pulmonary stenosis. However, each child may experience symptoms differently. Symptoms may include:
- Heavy or rapid breathing
- Shortness of breath
- Fatigue
- Rapid heart rate
- Swelling in the feet, ankles, face, eyelids and/or abdomen.
The symptoms of pulmonary stenosis may resemble other medical conditions or heart problems. The pediatric cardiologists at CHOC can carefully diagnose a suspected heart condition and provide a comprehensive treatment plan.
How is pulmonary stenosis diagnosed?
If a child’s doctor hears a heart murmur during a physical examination, the child will be referred to a pediatric cardiologist for a diagnosis. In this case, a heart murmur is simply a noise caused by the turbulence of blood flowing through the narrowed pulmonary valve. Symptoms your child exhibits will also help with the diagnosis.
A pediatric cardiologist specializes in the diagnosis and medical management of congenital heart defects, as well as heart problems that may develop later in childhood. The cardiologist will perform a physical examination, listen to the heart and lungs, and make other observations that help in the diagnosis. The location within the chest that the murmur is heard best, as well as the loudness and quality of the murmur (harsh or blowing) will give the cardiologist an initial idea of which heart problem your child may have. Diagnostic testing for congenital heart disease varies by the child’s age and clinical condition. Some tests that may be recommended include the following:
- Chest X-ray. A diagnostic test that uses X-ray beams to produce images of internal tissues, bones, and organs onto film. Learn more about X-rays.
- Electrocardiogram (ECG or EKG). A test that records the electrical activity of the heart, shows abnormal rhythms (arrhythmias), and detects heart muscle stress. Learn more about electrocardiogram.
- Echocardiogram (echo). A procedure that evaluates the structure and function of the heart by using sound waves recorded on an electronic sensor that produce a moving picture of the heart and heart valves. Learn more about echocardiogram.
How is pulmonary stenosis treated?
Specific treatment for pulmonary stenosis will be determined by your child’s doctor based on:
- The child’s age, overall health and medical history
- Extent of the condition
- The child’s tolerance for specific medications, procedures or therapies
- Expectations for the course of the condition
- The family’s opinion or preference.
Mild pulmonary stenosis often does not require treatment. Moderate or severe stenosis is treated with repair of the obstructed valve. Several options are currently available.
Some infants will be very sick, require care in the cardiovascular intensive care unit (CVICU) or neonatal intensive care unit (NICU) prior to the procedure, and could possibly even need repair of the pulmonary valve if the stenosis is severe. Others, who are exhibiting few symptoms, will have the repair scheduled on a less urgent basis.
Repair options include the following:
- Balloon dilation or valvuloplasty. An interventional cardiac catheterization procedure is the most common treatment choice. A small, flexible tube (catheter) is inserted into a blood vessel in the groin, and guided to the inside of the heart. The tube has a deflated balloon in the tip. When the tube is placed in the narrowed valve, the balloon is inflated to stretch the area open. This procedure may be used for valvar pulmonary stenosis or branch types of pulmonary stenosis. Children who have undergone balloon dilation may need to follow antibiotic prophylaxis for a specific period of time after discharge from the hospital. Learn more about interventional cardiac catheterization.
- Valvotomy. Valvotomy is the surgical release of scar tissue within the aortic valve leaflets that are preventing the valve leaflets from opening properly.
- Valvectomy (with or without transannular patch). Valvectomy is the surgical removal of the valve and is frequently accompanied by the placement of an outflow patch to improve blood flow from the right ventricle into the pulmonary artery. Once the individual reaches adulthood, the pulmonary valve may need to be replaced.
- Patch enlargement. Patches are used to enlarge the narrowed areas. In subvalvar pulmonary stenosis, an incision is made into the right ventricle, muscle causing the obstruction below the pulmonary valve is divided, and a patch is sewn into the cut edges of the right ventricle to enlarge the area below the pulmonary valve where the narrowing used to be. In supravalvar pulmonary stenosis, the narrowing is in the artery just beyond the pulmonary valve. Patches are sewn into this artery to enlarge its diameter and relieve the narrowing.
- Pulmonary valve replacement. Replacement of the pulmonary valve is a surgical procedure that is often recommended in adulthood in the case of leaky pulmonary valves. A tissue valve (pig or human) may be used. Children who have undergone a valve replacement will need to follow antibiotic prophylaxis throughout their life.
Learn more about heart surgery.
What is the long-term outlook after pulmonary stenosis repair?
Your child’s cardiologist may recommend that antibiotics be given to prevent bacterial endocarditis for a period of time following surgery and always for all valve replacements. Occasionally, repeat interventional cath lab procedures may be necessary during infancy and childhood to stretch the valve open. Replacement of the pulmonary valve may be recommended later during adolescence or early adulthood to prevent complications such as enlargement of the right ventricle, heart failure, and arrhythmias (irregular or fast heartbeats).
Regular follow-up care at a center offering pediatric or adult congenital cardiac care should continue throughout the individual’s lifespan.
Consult your child’s doctor regarding the specific outlook for your child.














