The Training Program
The doctoral internship in health service psychology training program at CHOC specifically focuses on the development of specialized professional skills in pediatric and child clinical psychology. We expect that interns will enter the program with previous experience in child psychotherapy and child assessment. During the year, interns will receive first-hand experience in applying their knowledge of child development and their skills as a child therapist to children with co-occurring medical and mental health conditions. Interns have the opportunity to do this through a wide variety of experiences, such as inpatient consultation-liaison services to a variety of medical specialty units, more intensive experiences with specific medical specialty teams, and outpatient psychotherapy. In addition, the internship is committed to providing appropriate and relevant services to culturally diverse families. As an intern, you will be exposed to a multicultural context that challenges the professional practice of even the most seasoned psychologists. Orange County offers a very culturally diverse population.
Interns at CHOC participate in a variety of training activities. Interns have the opportunity to receive both a breadth of experience with children with medical diagnoses and more traditional child psychopathology along with in-depth experiences with specific specialty medical teams. There are a variety of core training experiences that take place throughout the entire training year. Trainees participate in two six-month specialty rotations through an array of CHOC specialty services and clinics. Trainees also participate in up to three targeted three-month minor rotations. Each training experience is described below.
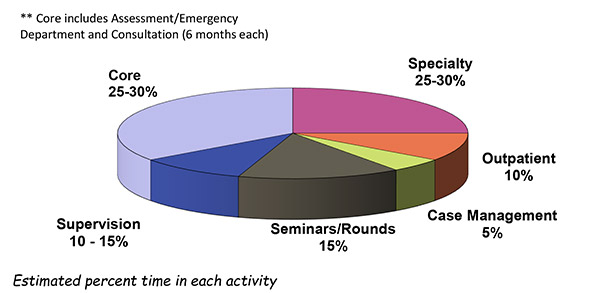
While time spent in each activity can differ on a week to week basis, the basic breakdown of time spent in each activity is as follows (chart based on 40 hour week):
Consultation-Liaison (CL) Service (6-month rotation): Breadth of experience with a variety of medical diagnoses comes from an intensive 6-month rotations with the consultation and liaison service at CHOC. Interns not only serve as consultants for the patient and/or family, but for the medical team, around a variety of issues. Consults are requested by attending physicians, residents, nurses, or other health care providers for children who are hospitalized for medical diagnoses and are experiencing concomitant psychological problems. Referral questions range from behavioral emergencies to suicide attempts requiring safety assessment to coping with an initial diagnosis to concerns for possible somatization disorders to adherence to complicated medical regimens to parental discipline to coping with death and dying issues. Medical diagnoses also run the gamut from diabetes to epilepsy to pain disorders to gastrointestinal disorders to autoimmune disorders to oncology to somatic presentations with unknown etiology. After an initial assessment, interventions may range from a referral for outpatient psychotherapy to referrals for psychological or neuropsychological assessment to interventions with the child and/or family while in the hospital to consultation and interventions with the medical team. Interns participate on a general consultation service one day a week with a faculty supervisor. Interns will learn to conduct a brief clinical evaluation, formulate an impression, and formulate disposition plans. While cases can be complex, interns always work with a supervising faculty member, are part of a consultation liaison team which includes psychology attendings, psychology postdoctoral fellows, and another psychology intern, and participate in weekly CL rounds. The CL team also includes child and adolescent psychiatry fellows and psychiatry attendings. It is a busy consultation service, so you will be able to see 2 or more cases per week on average while on the service. (Supervisors: Maleia Mathis, Ph.D., & Mery Taylor, Ph.D.)
Psychological Assessment Experience: All interns will participate in 6 months of assessment experience during the internship. Within the 6 months of the assessment rotation, interns will complete psychological diagnostic evaluations within our Thompson Autism and Neurodevelopmental Center (TANC) at CHOC Assessment Clinic for children 6 years and younger with suspected neurodevelopmental disorders. During the assessment core rotation, interns will complete 2 assessments per month. The TANC Assessment Clinic receives a wide variety of referrals regarding suspected neurodevelopment disorders, including autism, language disorder, ADHD, global developmental delay, and intellectual disability. Interns will participate in multidisciplinary assessment clinic, working with neurologists, developmental/behavioral pediatricians, speech therapists, and occupational therapists to assess and provide recommendations for children with NDD. At the end of the training year, all interns will have proficiency with a variety of assessment instruments, referral questions, ability to provide feedback to children and families, and the ability to recognize when to seek consultation. (Supervisors: Lauren Couch, Ph.D., Jina Jang, Ph.D., & Linda Sepulveda, Psy.D.)
Outpatient Therapy: Interns will participate in CHOC Psychology’s Medical Coping Clinic (MCC) as their outpatient therapy experience for the full 12-months. Medical Coping Clinic provides short-term therapy (4-10 sessions) to patients ages 8-18 who are experiencing an overlap between their medical conditions and mental health functioning. This rotation offers an opportunity to obtain experience with a wide variety of clinical presentations, as patients are referred to MCC from nearly every CHOC medical specialty, including Neurology, Endocrinology, Gastroenterology, Oncology, Pulmonology, and many others. One of the main goals of MCC is to reduce barriers to accessing mental health services for CHOC patients and services are provided to patients with all insurance types, in-person or via telehealth, and using interpreters or bilingual clinicians as needed. Interns will provide psychodiagnostic evaluations to patients referred to MCC, evaluate and provide same-day feedback to patient/family whether a) they are a good fit for MCC short-term therapy model (4-10 sessions), b) a referral to community clinic for longer-term services is most appropriate, c) patient does not currently require therapy services (CHOC Psychology can be on ‘stand by’ in case future needs arise), or d) some combination of a, b, and c, and provide short-term therapy (4-10 sessions) to patients deemed appropriate for MCC services. Patients are seen in MCC when there is a mental health condition related to medical diagnosis. Examples include: Adjusting to a new medical diagnosis, Increased depression, anxiety, etc. that are negatively impacting medical adherence, Overall medical adherence concerns, Trauma related to medical procedures, hospitalizations, etc., and Impact of living with a chronic medical condition on functioning (e.g. social/peer relationships, school reintegration, young adulthood milestones). Interns on this rotation will have the opportunity to coordinate care with multi-disciplinary teams of pediatricians, nurse practitioners, medical residents, social workers, case managers and resource specialists. (Supervisors: Anton Petrenko, Ph.D., Anita Saavedra, Psy.D., and Kristen Yule, Ph.D.)
Emergency Department (3 to 6-month rotation): Interns on the Emergency Department rotation will work in the Emergency Department (ED) with patients who are presenting with social, emotional, and/or behavioral issues. Interns will learn about the most common behavioral health concerns (e.g., suicidal ideation, aggressive behaviors) that present to the emergency department. In the ED, interns will participate in evaluations of children presenting in a psychiatric crisis and help to determine what level of care is needed (such as admission to an inpatient psychiatric unit or intensive outpatient services) and what are appropriate discharge recommendations. In the ED, interns will also participate in an evidence supported family-based intervention for children in crisis. Interns will work with a variety of health care providers, including physicians, residents, nurses, and case managers. There will be a particular focus on the use of Motivational Interviewing (MI) elements. (Supervisors: Vicky Bouche, Ph.D. and Meredith Dennis, Ph.D.)
Behavioral Emergency Services/On Call: A distinctive feature of our program is that all interns receive training in managing behavioral emergencies through the provision of consultation services to the CHOC Emergency Department and hospital inpatient medical units. Interns will also have the opportunity to take call 1-3 days throughout the training year for high-risk consults. Trainees are always paired with a faculty member for this coverage. High risk consults include assessment of suicide risk or acute mental status changes. Interns will conduct a brief clinical interview, provide crisis intervention and immediate disposition plans for patients with suicidal ideation, potentially aggressive behaviors, and possible psychosis. This training experience helps to increase your competence and comfort in assessing and managing behavioral emergencies.
Specialty Rotations
Specialty rotations are designed to be an in-depth experience within a specific area. By focusing on a single medical service for six months, interns have the opportunity to become an integral part of the medical team. Interns will play a central and vital role in providing assessment and psychosocial interventions and consulting with the medical team. Rotations may vary each year, but at least 4 of the following rotations will be offered each year.
Possible rotations may include:
- Consultation-Liaison
- Eating Disorders
- Endocrinology
- Feeding Disorders
- Integrated Primary Care
- Mental Health Inpatient Center
- Oncology
- Pulmonology And Gastroenterology
Interns on the Consultation-Liaison specialty rotation will gain greater breadth and depth of experience with medical consultation-liaison services within a hospital setting. The combination of the core rotation (above) and specialty rotation in consultation-liaison, would allow interns to work with a larger variety of medical diagnoses/presentations, participate in specialized follow-up sessions, conduct brief, targeted interventions, participate in team meetings and additional hospital meetings time permitting, and participate in medical rounding. Please see above description of CL core rotation for additional details (Supervisors: Maleia Mathis, Ph.D., & Mery Taylor, Ph.D.).
Interns on the Eating Disorders rotation spend one day per week within a pediatric inpatient medical setting at CHOC at Mission Hospital. Interns deliver services to children and adolescents admitted for medical stabilization for their eating disorder. The rotation includes conducting comprehensive initial intakes, as well as follow-up interventions for a variety of eating disorders including Anorexia Nervosa, ARFID, and Bulimia Nervosa. Furthermore, interns have the opportunity to develop skills in utilizing an Family-Based Treatment (FBT) approach within an inpatient setting (an evidence-based treatment for eating disorders). Interns provide parent and patient psychoeducation, individual therapy with parents and patients, and facilitation of group meals and group therapy. Interns are integrated into the Eating Disorders multidisciplinary team, which includes physicians, nurse practitioners, dieticians, social workers, case managers, and child life specialists (Supervisor: Katelyn Anderson, Ph.D).
Interns on the Endocrinology rotation will participate in the Endocrine Clinic (Type-I and Type-II Diabetes clinics), with a variety of health care providers including physicians, nurses, case managers, nutritionists, social workers, and diabetes nurse educators. Interns will play an integrated role in a multidisciplinary diabetes clinic by conducting depression screenings and providing same-day consultation upon referral. Interns will engage in conducting brief psychological screening for the purpose of identification of any mental health problems that may need further psychological assessment, ensure appropriate risk/safety assessment, and provide appropriate recommendations and referrals. Interns are expected to provide the endocrinologists with verbal feedback after screening a patient as well as complete a brief electronic report. Interns will also contribute their professional opinion and expertise in monthly psychosocial rounds and maintain involvement in ongoing program development initiatives (curriculum development for therapy and/or group protocols, community engagement and education, etc.). Interns also will have the opportunity to provide short-term outpatient treatment geared towards adherence interventions for patient’s screened/referred to psychology (Supervisor: Mercedes Palacios, Ph.D.).
Interns on the Feeding Disorders rotation will participate in multidisciplinary outpatient feeding evaluations within the CHOC Feeding team’s multidisciplinary outpatient evaluation clinic. This team includes physicians, nurse practitioners, speech therapists, occupational therapists, dieticians, and social workers. Interns will also participate in the innovative intensive 21-day inpatient feeding program. Common diagnoses for the inpatient feeding program include G-tube weaning and enhancing oral intake and variety (e.g., children with symptoms of ARFID). Interns will work closely with children and families participating in the observation of meals in a state of the art multi-media room and in providing behavioral interventions to the patients and parent training for the parents. Interns will work with both patients and parents during the inpatient admission. Additionally, interns will participate in outpatient multidisciplinary evaluations for children with feeding concerns and assist with assessment, behavioral observations, and providing appropriate recommendations. Interns on this rotation will gain knowledge about complex feeding disorders and techniques to treat feeding difficulties. Interns participate in program development and quality improvement endeavors as well. Interns also have the opportunity for co-treatment of complex feeding disorders in an outpatient psychology clinic (Supervisor: Cindy Kim, Ph.D., ABPP).
The Integrated Primary Care rotation aims to reduce barriers in accessing mental health services for a diverse and underserved population through integration into CHOC’s pediatric clinics throughout Orange County. This rotation offers the unique opportunity to be families’ first introduction to psychological services and will provide skill development in a fast-paced multidisciplinary environment through various clinical experiences. Interns will provide targeted mental health evaluations utilizing a “warm handoff” which may result in psychoeducation, skill building, and referrals to community mental health resources; provide brief outpatient follow-ups in clinic (30 minutes or less); co-lead psychoeducational groups targeted towards parents and patients in our primary care clinics; and work closely with the medical team to provide education, recommendations, and care coordination. Interns will acquire skills with regard to the evaluation of risk and safety concerns and safety planning within a primary care setting. Interns also will gain experience working with culturally and linguistically diverse patients across the developmental spectrum and develop a greater understanding about barriers to accessing care. Interns on this rotation will have the opportunity to work within a multi-disciplinary setting with a team of pediatricians, nurse practitioners, medical residents, social workers, case managers and resource specialists (Supervisor: Sarah Ruiz, Ph.D.).
The Mental Health Inpatient Center (MHIC) rotation: The Mental Health Inpatient Center (MHIC) is an acute psychiatric inpatient center with 18 private rooms and an outdoor play area serving children and adolescents ages 3-17. Many of these youths are hospitalized for concerns of suicidality, non-suicidal self-injurious behaviors, aggression, and psychosis. The intern on this rotation will receive clinical training in working with an interdisciplinary team for crisis stabilization facilitating evidence-based group therapy, conducting brief intake interviews, providing milieu interventions, and psychodiagnostics assessments. The intern may also see an individual case conducting brief, targeted individual as well as family therapy, safety planning, and discharge planning with the goal of increasing safety and linkage to appropriate aftercare services. Interns will acquire skills in crisis stabilization intervention, group therapy, and psychodiagnostic testing within the context of acute mental health. Interns will gain a general understanding of acute psychiatric hospitalization criteria of Danger to Self (DTS), Danger to Others (DTO), and Grave Disability (GD), as well as a specific understanding of acute as opposed to chronic risk in assessing for suicide rooted in Joiner’s Interpersonal Theory of Suicide Risk. Interns will have the opportunity to learn and apply evidence-based interventions within the context of group, milieu, individual and family therapy adapted for crisis management, utilizing CBT, DBT, ACT, and CAMS to address hospitalization criteria (Supervisor: Francesca Bahn, Ph.D.).
The Oncology rotation involves working with infants, children, and teens with many types of cancer and following them throughout their inpatient medical treatment and frequently beyond. Psychology has an important role in CHOC’s Oncology Program and supports patients and families across the care continuum. Often psychosocial services begin at, or shortly after diagnosis, and are available to patients and families as they navigate the unique challenges a cancer diagnosis, treatment, and survivorship present. Psychology interns have the opportunity to work closely with medical teams as part of the multidisciplinary care team to provide psychosocial and emotional support to oncology patients. Clinical opportunities may include conducting psychosocial assessments and screening and delivering evidence-based intervention and consultation. Patients may include those in active treatment, undergoing bone marrow transplants, patients on maintenance chemotherapy, and patients in survivorship. The Oncology rotation has a large interdisciplinary training aspect, as Psychology plays an important role within the Oncology Division, and is involved in ongoing coordination with physicians, nursing, and the other members of the Oncology Psychosocial Team (social workers, child life specialists, CHOC schoolteachers, and chaplains).
Interns on the Pulmonology and Gastroenterology rotation work closely with the multidisciplinary Pulmonary team, with a focus on patients with cystic fibrosis (CF), and the Gastroenterology (GI) Team. Interns will participate in multidisciplinary cystic fibrosis clinic and will conduct anxiety and depression screening in the outpatient medical clinic for patients with cystic fibrosis ages 12-21 years, as well as caregivers of patients birth to 18. As their primary role in clinic, interns will conduct a brief diagnostic interview to assess symptoms, distress, and impairment; provide psychoeducation about symptoms; offer tailored recommendations, including preventative interventions; and engage patients/families in motivational interviewing to build willingness to take steps toward implementing recommendations. Interns will also offer referrals and linkage to resources, as indicated. As a secondary activity, interns conduct brief assessments with infants, toddlers, and young children to assess mood and behavioral functioning; interns will learn to offer anticipatory or tailored guidance regarding management of procedural distress, interventions to reduce boredom/distress during lengthy CF treatments, and strategies to promote adjustment to CF, positive family relationships, and family communication. Interns on this rotation will have the opportunity to work within a multi-disciplinary setting with a team of pulmonologists, nurse practitioners, gastroenterologists, dieticians, respiratory therapists, physical therapists, case managers, and social workers.
Interns also will have the opportunity to consult within a functional abdominal pain GI clinic. As the psychological consultant in this clinics, interns will triage, assess for psychosocial factors impacting physical functioning, provide brief interventions, and conduct disposition planning within a fast-paced clinic setting. Interns receive training in cross-cutting issues in pediatric psychology, including adherence, pain, procedural anxiety/distress, family functioning, adjustment to illness, and depression/anxiety superimposed on chronic illness. Interns implement motivational interviewing techniques in both clinics to assist with providing psychoeducation, assessing readiness for change, and problem-solving around potential barriers to adherence (Supervisors: Adrianne Alpern, Ph.D. & Mery Taylor, Ph.D.).












