Epileptic Encephalopathy
What is Epileptic Encephalopathy?
Epileptic encephalopathy is the name used to describe severe cases of epilepsy that result in reduced cognitive and behavioral function.
Epileptic encephalopathy typically occurs early in a child’s life, starting in infancy, and can be characterized by generalized (abnormal activity in both halves of the brain) or focal seizures (starting in one part of the brain) that are recurrent, severe and often resistant to antiepileptic medications. Damage to the brain from the frequent seizure activity often leads to delays in development or the loss of developed skills. However, in some cases, a child’s development impairment can also be a result of the underlying condition causing the epilepsy. These conditions are referred to as Developmental Epileptic Encephalopathies (DEE) to acknowledge the presence of multiple causes for the developmental damages.
Epileptic Encephalopathy Syndromes
While encephalopathy can occur in any epileptic condition, there are eight severe epileptic syndromes that are commonly associated with epileptic encephalopathy. These conditions include:
- West Syndrome. Also known as infantile spasms, it is characterized by seizures that last a few seconds and occur in clusters (up to 150 seizures at a time). Some babies will experience up to 60 clusters in a day.
- Dravet Syndrome. Formerly called severe myoclonic epilepsy of infancy, this genetic condition is characterized by frequent, prolonged seizures that are commonly triggered by hyperthermia (high body temps). It typically begins within the first year of a child’s life.
- Early Myoclonic Encephalopathy (EME). Also referred to as neonatal myoclonic encephalopathy, this condition usually occurs in newborn infants. It is characterized by frequent drug resistant seizures that cause severe developmental damage resulting in reduced life expectancy.
- Continuous Spike Wave of Sleep (CSWS). This condition typically begins in children ages 2-12 years old and affects boys more often than girls. While various types of seizures are experienced within this syndrome, they all often result in a noticeable slowing of cognitive function 1-2 years after the seizure onset.
- Electrical Status Epileptics During Slow-Wave Sleep (ESES). While sometimes used interchangeably with CSWS, this condition is identified through the specific EEG pattern. As such, ESES can commonly be used to refer to the specific EEG abnormalities with CSWS reserved for the condition. Children who suffer from these epilepsies, experience epileptic activity during non-REM sleep that produces an EEG pattern of near continuous spike waves.
- EECSWS or epileptic encephalopathy with continuous spike-and-wave during sleep is a more specific term used describe children who suffer from cognitive, behavioral and psychiatric impairment as a result of their unique ESES pattern epileptic activity. It typically occurs in children 2-4 years old who experience infrequent seizures.
- Landau Kleffner Syndrome (LKS). Also called progressive epileptic aphasia, children with this syndrome typically experience focal motor seizures that occur infrequently during sleep and resolve with age. Along with seizures, children will experience a progressive loss of their ability to talk and understand speech.
- Ohtahara Syndrome. Sometimes referred to as early infantile epileptic encephalopathy (EIEE), these seizures typically begin around 3 months. They’re characterized by tonic spasms and focal seizures that are unresponsive to medication.
- Lennox-Gastaut Syndrome (LGS). In this severe form of epilepsy, children can suffer from multiple types of seizures with 1 out of 4 people exhibiting no underlying cause. While LGS usually persists through to adulthood, this condition is responsive to treatment that can help lessen seizures.
- Myoclonic Status in Nonprogressive Encephalopathies. Characterized by myoclonic seizures that occur in clusters, last for prolong periods (sometimes days), and are recurring. The majority of children with this syndrome have an underlying chromosomal disorder or structural/developmental brain abnormalities.
Epileptic syndromes can be distinguished by seizure type, age of onset, electroencephalograph changes (EEG) – which are particularly abnormal in epileptic encephalopathies – and associated development impact. Learn more about epilepsy.
What Causes Epileptic Encephalopathy?
While causes of epileptic encephalopathy are determined on an individual case-by-case basis, common underlying causes of epileptic encephalopathies include:
- Genetics. While not always inherited, genetic causes mean a seizure is a direct result of a genetic defect.
- Structural brain changes. When an abnormal structure, known to increase risk of seizures, is present in a child’s brain.
- Abnormal brain development. Cortical dysplasia and hypothalamic hamartoma are two developmental brain conditions that are known to cause seizures.
- Brain injury early in life. An external force to the head that causes the brain injury and results in seizures.
- Metabolic issues (less common). Metabolic issues can be the result of a blockage or underactivity of enzymes needed to metabolize food. Seizures can result from a buildup of toxins or the body’s inability to keep cells healthy.
Symptoms of Epileptic Encephalopathy
Symptoms of epileptic encephalopathy are largely dependent on the specific epileptic syndrome experienced. However, seizures associated with epileptic encephalopathy are typically very frequent, severe and often characterized by tonic, atonic, or myoclonic seizures.
- Tonic Seizures: Sudden stiffening or tension in the arm, leg, or trunk muscles that lasts about 20 seconds and often occurs during sleep.
- Atonic Seizures: A sudden loss of muscle strength. Also referred to as akinetic seizures, drop attacks or drop seizures.
- Myoclonic Seizures: Short, shock-like jerks that can occur in a single or group of muscles.
Additionally, EEGs of epileptic encephalopathy are commonly very irregular with diffuse slowing in the background (suggesting cerebral dysfunction) and frequent seizure discharges. And in some cases, EEGs conducted before or after the seizure onset show no abnormalities. Beyond frequent and severe seizures, the other most noticeable symptom that signal a child is suffering from epileptic encephalopathy is the presence of developmental delays or regression.
For more information on symptoms, review the common symptoms of epilepsy.
How is Epileptic Encephalopathy Diagnosed?
Diagnosis of epileptic encephalopathies occurs in three stages that work together to inform treatment planning. The diagnostic stages include identification of an underlying cause, evaluation of a child’s seizures, and discovery of other medical issues that need to be addressed.
Identification of the underlying cause
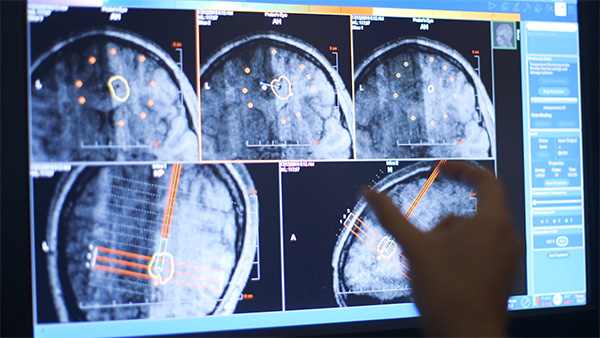
Identifying the underlying cause of a child’s epilepsy is the best way to determine the appropriate treatment. Diagnostic tests used to identify causes include electroencephalogram (EEG) and magnetic resonance imaging (MRI). Other tests that may be considered include genetic testing, metabolic tests on blood, urine, or spinal fluid. When seizures are located in a focal area of the brain, but an MRI is not sufficient in determining the exact location, a positron emission tomography (PET) or magnetoencephalography (MEG) may also be conducted.
Evaluation of seizure frequency and types
Families are responsible for providing doctors with a detailed history of their child’s seizures. This will include a description of seizures (video documentation if possible), duration, frequency, recognized triggers, and a description of behavior after seizures. A detailed account of your child’s medication intervention will also be requested, including if they’ve used medications, how often they’re needed. A prolonged EEG (with video) may be conducted to verify how many seizures a child experiences in a day and better classify the type of seizure.
Discovery of other medical issues
Children who experience epileptic encephalopathy are at a higher risk for experiencing other learning, behavioral and emotional disorders, as well as other medical complications. It’s important that a child receives the most comprehensive care, which includes treatment planning for all other medical conditions.
Treatment of Epileptic Encephalopathy
Treatment for epileptic encephalopathy is dependent on the underlying cause for a child’s seizures and is specific to each epilepsy syndrome. However typical treatments for epilepsy can include:
- Anti-Seizure Medications (ASMs). Epileptic encephalopathies are known to be medication resistant.
- Vagus Nerve Stimulation
- Ketogenic Diets
- Surgical Intervention (when the seizures are focal)
Other Considerations for Children with Epileptic Encephalopathy
Even in conditions where seizures eventually go away, any neurological impairments caused by the seizures will be permanent. As such, there are some common long-term complications as a result of epileptic encephalopathies.
- Intellectual disability resulting from the underlying cause of the epilepsy as well as damage from prolonged, frequent seizures.
- Movement disorders are a common co-condition occurring alongside epileptic encephalopathy. Not to be confused with abnormal movements during seizures. Learn more about movement disorders.
- Respiratory issues of aspiration and pneumonia are also common in children with epileptic encephalopathy that experience a limited ability to roll, tun, or raise the head or cough.
Comprehensive Epilepsy Program at CHOC
At CHOC, we believe that every child deserves the chance to have a childhood, that’s why our epileptic encephalopathy treatment goes beyond just minimizing a child’s seizures, with an aim of maximizing every child’s developmental potential. Our team of pediatric epilepsy experts work to find the underlying causes of cognitive and behavioral impairment to assess opportunities to stop or modify a child’s encephalopathy.
Our Comprehensive Epilepsy Program is a national leader in pediatric epilepsy care, offering cutting-edge diagnostics, innovative medical approaches and advanced surgical interventions from the nation’s foremost epilepsy experts. When it comes to treatment for Epileptic Encephalopathy our team of experts is Learn more about our Comprehensive Epilepsy Program or see a CHOC Epileptologist today.

FAQs about Epileptic Encephalopathy
Epileptic Encephalopathy Clinical Trials at CHOC
At CHOC, we are dedicated to providing patients the very latest breakthrough treatments available to children, adolescents and young adults. Our efforts bring hope to patients with rare conditions, or conditions not responding to traditional treatments. Learn more about epilepsy research at CHOC.
We are currently participating in a clinical trial looking at drug intervention for children with EE-CSWS. Contact us to learn more about epileptic encephalopathy clinical trials at CHOC.












