 What is Crohn’s disease?
What is Crohn’s disease?
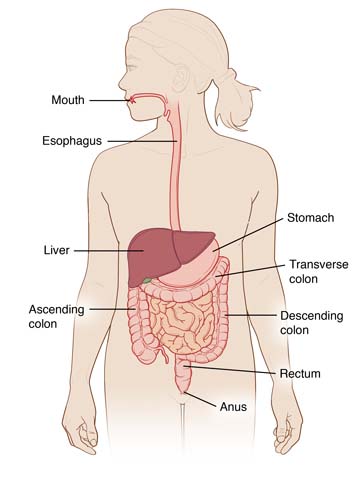
Crohn’s disease is type of inflammatory bowel disease (IBD). It is a chronic condition that may recur at various times over a lifetime. It usually involves the small intestine, most often the lower part called the ileum. In some cases, both the small and large intestine are affected. Inflammation may affect one or more locations in the digestive tract, including the mouth, esophagus, stomach, small intestine, large intestine, appendix and anus.
What causes Crohn’s disease?
No one knows for sure what causes Crohn’s disease or why it shows up when it does. We do know that people who have a family member with IBD are more likely to develop Crohn’s disease. One theory suggests that something, perhaps a virus or bacteria, affects the body’s immune system and triggers an inflammatory reaction in the intestinal wall. There is evidence that patients with this disease have abnormalities of the immune system. It is not known, however, whether the immune problems are a cause or a result of the disease. Nutrition may also play a role in the cause of Crohn’s disease.
Who is affected by Crohn’s disease?
While Crohn’s disease may affect people of all ages, the age group most often affected is 15 to 35 years. Crohn’s may also be seen in young children. Males and females are affected equally. It appears to run in some families, with about 20 percent of people with Crohn’s disease having a blood relative with some form of inflammatory bowel disease.
What are the symptoms of Crohn’s disease?
The following are the most common symptoms for Crohn’s disease. However, each child may experience symptoms differently. Symptoms may include:
- Abdominal pain, often in the lower right area
- Diarrhea, sometimes bloody
- Rectal bleeding
- Decreased appetite
- Decreased energy
- Fever
- Weight loss
- Failure to grow
- Rash
- Joint pain
- Canker sore in the mouth
- Persistent fissure, sore or opening in the skin in or around the anus.
Crohn’s disease may develop very slowly in some people with mild symptoms that may exist for years before diagnosis. After diagnosis, some people may have long periods of remission when they are free of symptoms, sometimes lasting for years. It may be difficult to predict when a remission may occur or when symptoms will return. It is important to get care from a physician experienced in diagnosing and caring for IBD. The symptoms of Crohn’s disease may resemble other conditions or medical problems. It is important to get a proper diagnosis from a doctor who specializes in treating pediatric gastrointestinal conditions.
How is Crohn’s disease diagnosed?
Children and adolescents who have experienced chronic abdominal pain, diarrhea, fever, weight loss, growth failure and anemia may be examined for signs of Crohn’s disease. In addition to a complete medical history and physical examination, diagnostic procedures for Crohn’s disease may include:
- Blood tests. These tests help doctors look for anemia or chronic inflammation. They also show any changes in the child’s protein, vitamin and mineral levels. Sometimes blood tests can help distinguish between ulcerative colitis and Crohn’s disease. Learn more about blood tests at CHOC.
- Stool tests. These tests look for evidence of blood loss or inflammation in the stool, or an infection by a parasite or bacteria causing the symptoms. Learn more about stool tests.
- Esophagogastroduodenoscopy (EGD or upper gastrointestinal endoscopy). A procedure in which a flexible scope is inserted through the mouth so that the child’s doctor can see abnormal growths, narrowing, inflamed tissues, ulcers and bleeding sites in the lining of the throat, esophagus, stomach and the beginning of the small intestine. During an endoscopy, doctors can also treat areas that are bleeding and take very tiny biopsies of tissues they would like to test. Learn more about endoscopy.
- Colonoscopy. A procedure in which a flexible scope inserted through the anus allows the doctor to see abnormal growths, narrowing, inflamed tissues, ulcers, polyps and bleeding sites in the lining of the large intestine and the final portion of the small intestine (distal terminal ileum). During a colonoscopy, the doctor can treat areas that are bleeding, remove polyps and take very tiny biopsies of tissues they would like to test. Learn more about colonoscopy.
- Push enteroscopy (push-pull enteroscopy or double balloon enteroscopy). A procedure that allows the doctor to see the small intestine that cannot be reached with traditional esophagogastroduodenoscopy. It is performed similar to an EGD. Biopsies can be taken during this study.
- Capsule endoscopy. A procedure that lets doctors see the parts of the small intestine that cannot be reached with traditional esophagogastroduodenoscopy. A video capsule is swallowed or placed in the intestine using an endoscope and passes through the intestine taking many pictures that can be compiled into a video. Biopsies cannot be taken during this study. Learn more about capsule endoscopy.
- Biopsy. Tiny, painless samples of tissue taken from the lining of the intestine for examination under a microscope in a laboratory. The samples are used to find abnormalities that cannot be seen with the naked eye and help determine more information about a patient’s disease. Taking a biopsy sample does not mean that the physician suspects a diagnosis of cancer.
- Upper gastrointestinal series (UGI, upper GI, barium swallow). An X-ray that creates images of the organs of the upper part of the digestive system: the esophagus, stomach and duodenum (the first section of the small intestine). A fluid called barium (a chalky liquid) is swallowed and coats the inside of the intestine so that it will show up on the X-ray. This test is used to look at the anatomy and movement of the intestine. It is does not show abnormalities in the lining of the intestine as well as endoscopy. Sedation is not used for this test. Learn more about X-rays.
- Upper gastrointestinal series with small bowel follow through (UGI w SBFT). A test that creates images of the organs of the upper part of the digestive system including the entire small intestine (not just the first section). A fluid called barium (a chalky liquid) is swallowed and coats the inside of the intestine so that it will show up on the X-ray. This test is used to look at the anatomy and movement of the intestine. It does not show abnormalities in the lining of the intestine as well as endoscopy. Sedation is not used for this test. Learn more about X-rays.
- Computed tomography enterography (CT of abdomen and pelvis, CTE). An X-ray of the intestine that gives a three dimensional view of the belly including the intestine and structures surrounding the intestine. This test uses oral and IV contrast and usually does not require sedation. Learn more about CT.
- Magnetic resonance enterography (MRI of abdomen and pelvis, MRE). An imaging test of the intestine that gives a three-dimensional view of the belly including the intestine and structures surrounding the intestine. This test uses oral and IV contrast and may require sedation, depending upon the age of the patient. Learn more about MRI.
- Barium enema. An X-ray test that examines the organs of the lower part of the digestive system: the terminal ileum, colon and anus. Barium or another form of contrast is given through the anus as a controlled enema. This test is used to evaluate the anatomy and movement of the intestine. It may show strictures (narrowed areas) and obstructions (blockages) of the large intestine. It does not show abnormalities in the lining of the intestine as well as colonoscopy. Sedation is not used for this test. Learn more about X-rays.
What is the treatment for Crohn’s disease?
At this time there is no cure for Crohn’s disease. However, there are things that can be done to help control Crohn’s disease. At CHOC, treatment plans are developed based on each patient’s unique medical, physical, social and emotional needs.
The goals of treatment may include:
- Correcting nutritional deficiencies
- Controlling inflammation
- Supporting optimal growth and weight gain
- Reducing symptoms so your child can live a more normal life.
Specific treatment is determined by your child’s doctor based on the following:
- The child’s age, overall health and medical history
- The extent and location of the Crohn’s disease
- The child’s tolerance for specific medications, procedures or therapies
- The family’s opinion or preference.
Treatment may include:
Medication therapy. Your child’s gastroenterologist may recommend one or a combination of medications that will help the intestine heal. The classes of medications available include aminosalicyclates, antibiotics, corticosteroids, immunomodulators and biologic therapies.
Diet and vitamin supplements. No special diet has been proven effective for preventing or treating Crohn’s disease. No specific food can be blamed as the cause of Crohn’s disease. Good nutrition should be one important part of a complete treatment plan. Vitamin and mineral supplements can be very important in the healing process, especially iron, zinc, calcium and vitamin D. Probiotics may be an important addition to help control symptoms.
Children with Crohn’s disease may lose weight because they are not getting enough calories because:
- They may avoid eating to prevent pain that comes with digestion.
- They may absorb nutrients poorly through the inflamed digestive tract.
- They have greater nutritional needs than average because of their disease.
- They may not be enthusiastic about eating when favorite foods are eliminated from their diet.
Some dietary changes may help control symptoms. In some cases symptoms are made worse by milk, alcohol, hot spices or fiber, but this may not be true for everyone. Large doses of vitamins are not an effective treatment and may even cause harmful side effects. Our gastroenterologist and dietitian can work with patients and families to determine possible foods to avoid and foods to emphasize.
The use of nutritional therapies as a sole treatment for Crohn’s disease is a controversial topic that needs discussion on a case-by-case basis. Nutritional supplements or special high-calorie liquid formulas may sometimes be suggested. It is rare, but possible, that a patient will need intravenous (by vein) feeding to support their nutrition during challenging stages of their treatment plan. Learn more about total parenteral nutrition (TPN).
Hospitalization. Children with Crohn’s disease are sometimes sick enough to require hospitalization to correct anemia and malnutrition and to stop diarrhea, vomiting and loss of blood, fluids, and mineral salts. Patients may need a special diet, feeding through a vein, medications or, in rare cases, surgery.
Surgery. Crohn’s disease may be helped by surgery, but is not likely to be cured by surgery. Inflammation tends to return to the areas of the intestine next to the area that has been removed. Any surgical intervention in Crohn’s disease must be approached with caution. However, surgery may help relieve chronic symptoms of active disease that do not respond to medical therapy or to correct complications, such as intestinal blockage, perforation, abscess, fistula or bleeding. Types of surgery include:
- Drainage of abscesses.
- Removal of a section of bowel due to blockage, stricture or fistula. This type of surgery may result in a shortened bowel that requires additional nutrition support.
- Ostomy. Some people must have part of their intestines removed and a new method of removing the stool from the body is created. The surgery to create the new opening is called ostomy and the new opening is called a stoma.
The type of ostomy performed depends on how much and which part of the intestines are removed, and may include:
- Ileostomy. The colon and rectum are removed and the bottom part of the small intestine (ileum) is attached to the stoma.
- Colostomy. Part of the colon is removed or bypassed and a small portion of the colon is brought up to the surface of the skin to create the stoma. Sometimes, a temporary colostomy may be performed when part of the colon has been removed and the rest of the colon needs to heal.
- Ileoanal reservoir surgery (J-pouch among other terms). This is an alternative to a permanent ileostomy and uses part of the small intestine to create a pouch near the rectum to hold stool for evacuation at a later time. The muscle of the rectum is left in place, so the stool in the pouch does not leak out of the anus. People who have this surgery are able to control their bowel movements. This surgery is more common in ulcerative colitis patients but may be necessary in Crohn’s disease patients.
Learn more about surgery at CHOC.
What is the long-term outlook for a child with Crohn’s disease?
Crohn’s disease is a chronic condition that may recur or flare at various times over a lifetime. Children may experience physical, emotional, social and family problems as a result of the disease, increasing the importance of proper management and treatment of the condition at a long-term, comprehensive program like the IBD Program at CHOC.
The following chart summarizes some of the problems children may face.
| Emotional Responses | Social Problems | Effects on the Family |
|
|
|
At CHOC our multidisciplinary team includes a dedicated dietitian, social worker and case manager who work with families and patients to make life with Crohn’s disease more manageable. Our psychology department is readily available to help patients deal with chronic illness and develop the skills it takes to cope on their own in daily life. Our team provides easy access to all our resources including office visits, group teaching sessions and educational materials.












