What is a ventricular septal defect?
 A ventricular septal defect is an opening in the ventricular septum, or dividing wall between the two lower chambers of the heart known as the right and left ventricles. VSD is a congenital (present at birth) heart defect. As the fetus is growing, something occurs to affect heart development during the first eight weeks of pregnancy, resulting in a VSD.
A ventricular septal defect is an opening in the ventricular septum, or dividing wall between the two lower chambers of the heart known as the right and left ventricles. VSD is a congenital (present at birth) heart defect. As the fetus is growing, something occurs to affect heart development during the first eight weeks of pregnancy, resulting in a VSD.
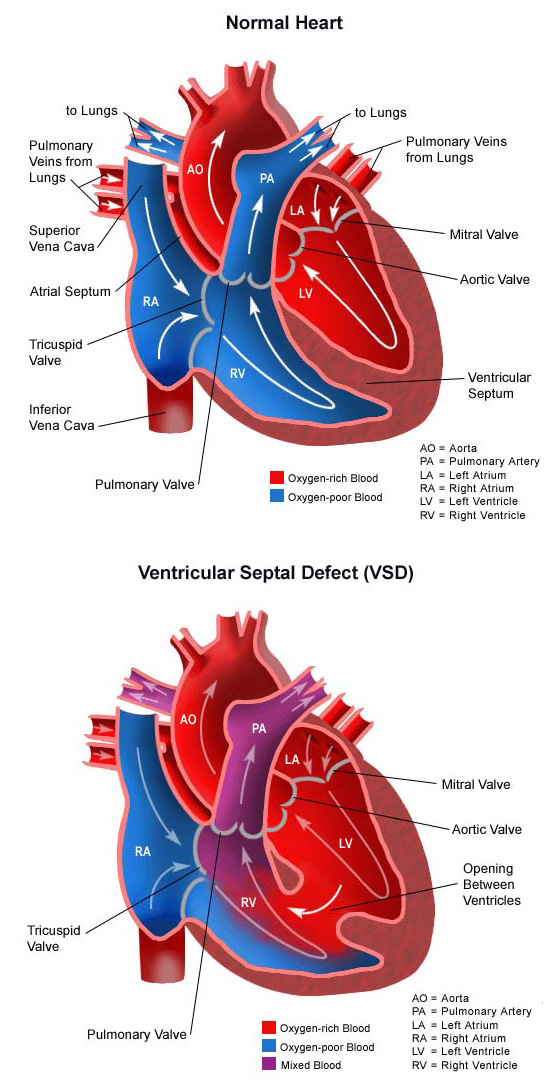
Normally, oxygen-poor (blue) blood returns to the right atrium from the body, travels to the right ventricle, then is pumped into the lungs where it receives oxygen. Oxygen-rich (red) blood returns to the left atrium from the lungs, passes into the left ventricle, and then is pumped out to the body through the aorta.
A ventricular septal defect allows oxygen-rich (red) blood to pass from the left ventricle, through the opening in the septum, and then mix with oxygen-poor (blue) blood in the right ventricle.
What are the different types of VSD?
There are four basic types of VSD:
- Membranous VSD. An opening in a particular area of the upper section of the ventricular septum (an area called the membranous septum), near the valves. This type of VSD is the most commonly operated on since most membranous VSDs do not usually close spontaneously.
- Muscular VSD. An opening in the muscular portion of the lower section of the ventricular septum. This is the most common type of VSD. A large number of these muscular VSDs close spontaneously and do not require surgery.
- Atrioventricular canal type VSD. A VSD associated with atrioventricular canal defect. The VSD is located underneath the tricuspid and mitral valves.
- Conal septal VSD. The rarest of VSDs which occur in the ventricular septum just below the pulmonary valve.
Ventricular septal defects are the most commonly occurring type of congenital heart defect, accounting for about half of congenital heart disease cases.
What causes ventricular septal defect?
The heart is forming during the first eight weeks of fetal development. It begins as a hollow tube, then partitions within the tube develop that eventually become the septa (or walls) dividing the right side of the heart from the left. Ventricular septal defects occur when the partitioning process does not occur completely, leaving an opening in the ventricular septum.
Some congenital heart defects may have a genetic link, either occurring due to a defect in a gene, a chromosome abnormality, or environmental exposure, causing heart problems to occur more often in certain families. Most ventricular septal defects occur sporadically (by chance), with no clear reason for their development.
Why is ventricular septal defect a concern?
If not treated, this heart defect can cause lung disease. When blood passes through the VSD from the left ventricle to the right ventricle, a larger than normal volume of blood must be handled by the right side of the heart. Extra blood then passes through the pulmonary artery into the lungs, causing higher pressure than normal in the blood vessels in the lungs.
A small opening in the ventricular septum allows a small amount of blood to pass through from the left ventricle to the right ventricle. A large opening allows more blood to pass through and mix with the normal blood flow in the right heart. Extra blood causes higher pressure in the blood vessels in the lungs. The larger the volume of blood that goes to the lungs, the higher the pressure will be.
The lungs are able to cope with this extra pressure for a while, depending on exactly how high the pressure is. After a while, the blood vessels in the lungs become diseased by the extra pressure.
As pressure builds up in the lungs, the flow of blood from the left ventricle, through the VSD, into the right ventricle, and on to the lungs will diminish. This helps preserve the function of the lungs, but causes yet another problem. Blood flow within the heart goes from areas where the pressure is high to areas where the pressure is low. If a ventricular septal defect is not repaired, and lung disease begins to occur, pressure in the right side of the heart will eventually exceed pressure in the left. In this instance, it will be easier for oxygen-poor (blue) blood to flow from the right ventricle, through the VSD, into the left ventricle, and on to the body. When this happens, the body does not receive enough oxygen in the bloodstream to meet its needs.
Some ventricular septal defects are found in combination with other heart defects (such as in transposition of the great arteries).
What are the symptoms of a ventricular septal defect?
The size of the ventricular septal opening will affect the type of symptoms noted, the severity of symptoms and the age at which they first occur. A VSD permits extra blood to pass from the left ventricle through to the right side of the heart, and the right ventricle and lungs become overworked as a result. The larger the opening is, the greater the amount of blood that passes through and overloads the right ventricle and lungs.
Symptoms often occur in infancy. The following are the most common symptoms of VSD. However, each child may experience symptoms differently. Symptoms may include:
- Fatigue
- Sweating
- Rapid breathing
- Heavy breathing
- Congested breathing
- Disinterest in feeding, or tiring while feeding
- Poor weight gain.
The symptoms of VSD may resemble other medical conditions or heart problems. Always consult your child’s doctor for a diagnosis.
How is a ventricular septal defect diagnosed?
Your child’s doctor may have heard a heart murmur during a physical examination, and referred your child to a pediatric cardiologist for a diagnosis. A heart murmur is simply a noise caused by the turbulence of blood flowing through the opening from the left side of the heart to the right.
A pediatric cardiologist specializes in the diagnosis and medical management of congenital heart defects, as well as heart problems that may develop later in childhood. The cardiologist will perform a physical examination, listen to the heart and lungs, and make other observations that help in the diagnosis. The loudness and quality of the murmur (such as, harsh or blowing) as well as the location within the chest where the murmur is heard best, will give the cardiologist an initial idea of which heart problem your child may have. The type of diagnostic testing used to diagnose a heart condition is determined by the child’s age and clinical condition. Some tests that may be recommended include the following:
- Chest X-ray. A diagnostic test that uses X-ray beams to produce images of internal tissues, bones and organs onto film. With a VSD, the heart may be enlarged because the right ventricle handles larger amounts of blood flow than normal. Also, there may be changes that take place in the lungs due to extra blood flow that can be seen on an X-ray. Learn more about chest X-ray.
- Electrocardiogram (ECG or EKG). A test that records the electrical activity of the heart, shows abnormal rhythms (arrhythmias) and detects heart muscle stress. Learn more about electrocardiogram.
- Echocardiogram (echo). A procedure that evaluates the structure and function of the heart by using sound waves recorded on an electronic sensor that produce a moving picture of the heart and heart valves. An echo can show the pattern of blood flow through the septal opening, and determine how large the opening is, as well as much blood is passing through it. Learn more about echocardiogram.
How is ventricular septal defect treated?
Specific treatment for VSD will be determined by your child’s doctor based on:
- The child’s age, overall health and medical history
- Extent of the disease
- The child’s tolerance for specific medications, procedures, or therapies
- Expectations for the course of the defect
- The family’s opinion or preference.
Small ventricular septal defects usually close spontaneously as your child grows. A larger VSD usually requires surgical repair. Regardless of the type, once a ventricular septal defect is diagnosed, your child’s cardiologist will evaluate your child periodically to see whether it is closing on its own. A VSD will be repaired if it has not closed on its own to prevent lung problems that will develop from long-time exposure to extra blood flow. Treatment may include:
- Medical management. Some children have no symptoms, and require no medication. However, some children may need to take medications to help the heart work better, since the right side may be under strain from the extra blood passing through the VSD. Medications that may be prescribed include the following:
– Diuretics. The body’s water balance can be affected when the heart is not working as well as it could. These medications help the kidneys remove excess fluid from the body.
– ACE inhibitors. Medications that lower the blood pressure in the body, making it easier for the blood to be pumped from the left ventricle into the body (because of its lowered blood pressure) rather than that blood being pumped from the left ventricle across the VSD into the right ventricle then into the lungs. - Adequate nutrition. Infants with a larger VSD may become tired when feeding, and are not able to eat enough to gain weight. Options that can be used to ensure your baby will have adequate nutrition include the following:
– High-calorie formula or breast milk. Special nutritional supplements may be added to pumped breast milk or formula that increase the number of calories in each ounce, thereby allowing your baby to drink less and still take in enough calories to grow properly.
– Supplemental tube feedings. Feedings given through a small, flexible tube that passes through the nose, down the esophagus, and into the stomach, can either supplement or take the place of breast or bottle feedings. Infants who can drink part of their feeding, but not all, may be fed the remainder through the feeding tube. Infants who are too tired to breast or bottle feed may receive their breast milk or formula through the feeding tube alone. - Surgical repair. The goal is to repair the septal opening before the lungs become diseased from too much blood flow and pressure. Your child’s cardiologist will recommend when the repair should be performed based on echocardiogram and (less commonly) cardiac catheterization results. The operation is performed under general anesthesia. Depending on the size of the heart defect and your doctor’s recommendations, the ventricular septal defect will be closed with stitches or a special patch. Consult your child’s cardiologist for more information. Learn more about heart surgery.
- Interventional cardiac catheterization. In certain circumstances, your child’s VSD may be repaired by a cardiac catheterization procedure. One method currently being used to close some small muscular VSDs is the use of a device called a septal occluder. During this procedure, the child is sedated and a small, thin flexible tube is inserted into a blood vessel in the groin and guided into the heart. Once the catheter is in the heart, the cardiologist will pass the septal occluder across the VSD. The septal occluder closes the ventricular septal defect providing a permanent seal. Learn more about interventional cardiology.
What is the long-term outlook after VSD repair?
Most children who have had a ventricular septal defect repair will live normal, healthy lives. Activity levels, appetite and growth will return to normal in most children. Your child’s cardiologist may recommend that antibiotics be given to prevent bacterial endocarditis for a specific time period after discharge from the hospital.
Outcomes also depend on the type of VSD, as well as how early in life the VSD was diagnosed and whether or not it was repaired. With early diagnosis and repair of a VSD, the outcome is generally excellent, and minimal follow-up is necessary. When a VSD is diagnosed later in life, if complications occur after surgical closure, or the VSD is never repaired, the outlook may be poor. There is a risk for developing irreversible pulmonary hypertension (high blood pressure in the blood vessels of the lungs) or Eisenmenger’s syndrome. These individuals should receive follow-up care at a center that specializes in congenital heart disease.
Consult your child’s doctor regarding the specific outlook for your child.














