Understanding Transesophageal Echocardiogram
What is a transesophageal echocardiogram?
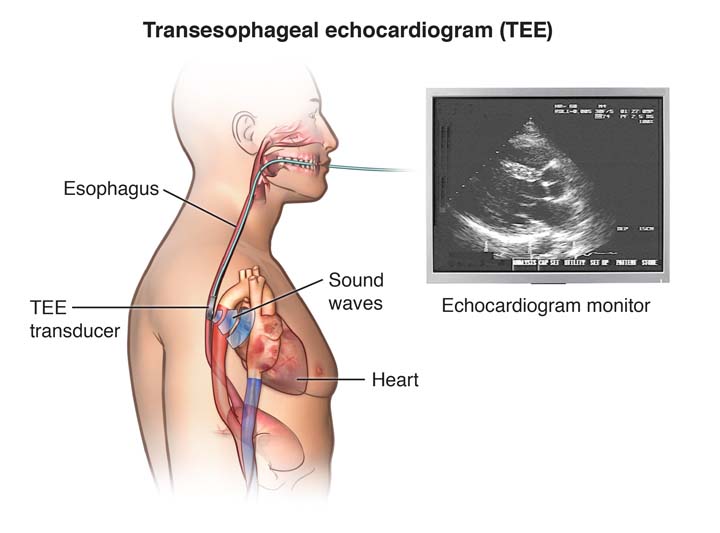
A transesophageal echocardiogram (TEE) is a diagnostic procedure used to assess the heart’s structure and function (a heart ultrasound). Just like a traditional transthoracic echocardiogram, a transducer sends out ultrasonic sound waves at a frequency too high to be heard. When the transducer is placed at certain locations and angles, the ultrasonic sound waves move through the skin and other body tissues to the heart tissues, where the waves bounce or “echo” off of the heart structures. The transducer picks up the reflected waves and sends them to a computer. The computer displays the echoes as images of the heart walls and valves.
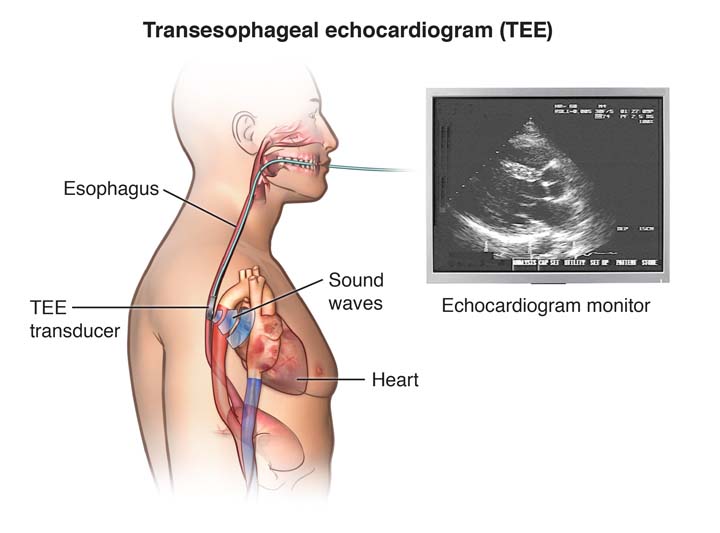
A TEE is performed by inserting a probe with a transducer down the esophagus, rather than placing the transducer on the chest as in a standard transthoracic echocardiogram (TTE). Because the probe is in the esophagus which is located right behind the heart, TEE provides a clearer images.
Certain conditions of the heart, such as valve disorders, implanted prosthetic (artificial) heart valves, and blood clots or masses inside the heart, are often better seen with TEE.
TEE is usually used during heart surgery to further assess the heart structure and function both before and after the operation to help optimize the heart surgery and make it safer.
Like a TTE, TEE may utilize one or more of several special types of echocardiography, including M-mode, Doppler, color Doppler, as well as 2-D (two-dimensional) and 3-D (three-dimensional) technologies.
What are the risks of the transesophageal echocardiogram?
 Possible risks associated with a transesophageal echocardiogram include, but are not limited to, the following:
Possible risks associated with a transesophageal echocardiogram include, but are not limited to, the following:
- Breathing problems
- Heart rhythm problems
- Infection
- Bleeding
- Injury to the esophagus, throat or inside of the mouth.
Patients with known problems of the esophagus, such as esophageal varices, esophageal obstruction or radiation therapy to the area of the esophagus should be evaluated carefully by the doctor before having the procedure.
There may be other risks depending upon a child’s specific medical condition or health history. Be sure to discuss any concerns with the child’s doctor prior to the procedure.
CHOC is accredited by the Intersocietal Accreditation Committee for pediatric transesophageal echocardiogram. IAC accreditation ensures a commitment to the quality of health care provided to patients.
What happens before a transesophageal echocardiogram?
- Before the procedure, the child’s doctor will explain the procedure and provide family members and the patient the opportunity to ask questions.
- The child’s legal guardian will be asked to sign a consent form that gives the doctor permission to do the test. It is important to read the form carefully and ask questions if something is not clear.
- The patient will need to fast (not eat or drink) for a certain period of time prior to the procedure. (This is often referred to as “NPO.”) The child’s doctor will provide specific guidelines. Learn more about NPO at CHOC.
- Parents should notify their child’s doctor if the child is allergic to or sensitive to medications, local anesthesia or latex. It is also important to tell the child’s doctor about all medications (prescription and over-the-counter) and herbal supplements the child may be taking, and if the child has a history of bleeding disorders, takes any anticoagulant (blood-thinning) medications, or other medications that affect blood clotting. The child’s doctor will provide instruction on which medications and supplements can and cannot be taken prior to the procedure.
- Prior to the TEE, the doctor may request a blood test prior to determine how long it takes for the child’s blood to clot. Other blood tests may be done as well.
- Patients are given sedative prior to the procedure to help them relax.
- Based on the child’s medical condition, other preparations may need to made before the procedure.
What happens during a transesophageal echocardiogram?
A TEE may be performed on an outpatient basis or as part of a stay in at CHOC. Procedures may vary depending on the child’s specific condition.
All patients are admitted to the Tidwell Procedure Center at CHOC. After being taken to a preoperative room, the child will:
- Remove jewelry or other objects that may interfere with the procedure.
- Remove clothing and put on a hospital gown.
- Use the restroom.
- Have an intravenous (IV) line placed in their hand or arm prior to the procedure so that medications and fluids can be given to the child as needed. The child is given a sedative through the IV that will help them feel more relaxed.
Once the child has been prepared for surgery, the doctor will answer any last minute questions before the child is taken to the operating room for the TEE. An anesthesiologist will usually assist with this procedure.
Once inside the room, the child lies on a bed. A pillow or wedge may be placed behind the child’s back for support and the child is connected to a cardiorespiratory monitor that records the electrical activity of the heart and monitors the heart during the procedure using small, adhesive electrodes. The child’s vital signs (heart rate, blood pressure, breathing rate and oxygenation level) are also monitored during the procedure. Some patients may also receive oxygen through nasal tubes.
After making sure the child is properly positioned and connected to the monitoring equipment, a local anesthetic spray is applied to the back of the throat. This spray numbs the back of the throat and makes passing the TEE probe more comfortable.
When the procedure begins, the TEE probe is very carefully passed through the child’s mouth and down the throat by the cardiologist. Once the probe is in the right place, the doctor will be able to see images of the structure of the child’s heart. After the necessary images are obtained, the probe is removed from the child’s throat. The procedure usually takes 20-30 minutes, depending on the child’s specific condition.
What happens after a transesophageal echocardiogram procedure?
After the procedure, the child is moved to the recovery area of the Tidwell Procedure Center. It is also referred to as the “PACU.” There, nurses monitor the child’s heart rate, ECG, blood pressure and oxygen levels. Once the child is alert, their gag reflex has returned and vital signs are normal, the ECG electrode pads, the oxygen probe and the IV will be removed. A nurse will let the child’s parents know when they can see them in the recovery area.
Some children may feel weak, tired or groggy for the remainder of the day of the procedure, and should feel normal by the day after the procedure. The patient’s voice maybe horse and/or their throat may be sore for a few days following the procedure due to the insertion of the TEE probe. This is normal but if it persists or worsens the child may need to be evaluated by a doctor.
Usually, children under the age of 1 year will be admitted to the hospital overnight to the cardiovascular intensive care unit (CVICU) for monitoring, while most other children can go home the same day.
The child should be able to resume his or her regular diet and activities the same or next day unless the doctor advises differently.
Generally, there is no special type of care following a TEE. However, the child’s doctor may have additional or alternate instructions after the procedure, depending on the child’s particular situation.
 Possible risks associated with a transesophageal echocardiogram include, but are not limited to, the following:
Possible risks associated with a transesophageal echocardiogram include, but are not limited to, the following:











