 What causes gastroparesis?
What causes gastroparesis?
Most often, this condition is a complication of type 1 diabetes. It can also occur in persons with type 2 diabetes, although not as frequently. Gastroparesis is caused when the vagus nerve, which controls the movement of food through the digestive tract, is damaged or stops working. When this happens, the movement of food is slowed down or stopped. The vagus nerve becomes damaged in people with diabetes when blood glucose (sugar) levels remain high over a long period of time.
Other causes of gastroparesis include the following:
- Anorexia nervosa
- Surgery on the stomach or vagus nerve
- Postviral syndromes
- Certain medications, particularly those that slow contractions in the intestine
- Disorders involving smooth muscle, such as amyloidosis and scleroderma
- Diseases of the nervous system, such as abdominal migraine
- Metabolic disorders, including hypothyroidism.
What are the symptoms of gastroparesis?
The following are the most common symptoms of gastroparesis. However, each individual may experience symptoms differently. Symptoms may include:
- Nausea
- Vomiting
- Weight loss
- Feeling full early when eating
- Abdominal bloating and/or discomfort (epigastric pain)
- Heartburn.
The symptoms of gastroparesis may resemble other medical conditions or problems. Always consult your child’s doctor for a diagnosis.
How is gastroparesis diagnosed?
In addition to a complete medical history and physical examination, diagnostic procedures for gastroparesis may include the following:
- Blood tests. These tests check blood counts and measure chemical and electrolyte levels. Learn about blood tests at CHOC.
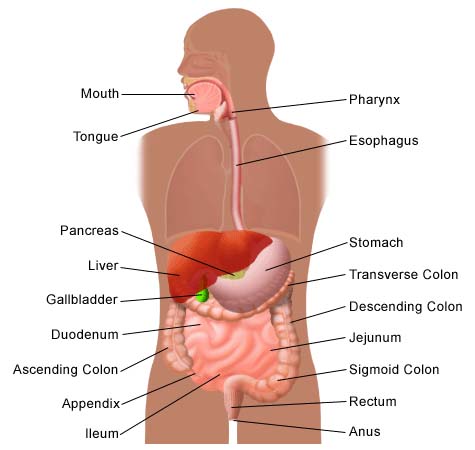
- Upper GI (gastrointestinal) series (also called barium swallow). An X-ray diagnostic test that examines the organs of the upper part of the digestive system: the esophagus, stomach, and duodenum (the first section of the small intestine). A fluid called barium (a metallic, chemical, chalky, liquid used to coat the inside of organs so that they will show up on an X-ray) is swallowed. X-rays are then taken to evaluate the digestive organs. Learn more about X-rays at CHOC.
- Gastric manometry. This test measures electrical and muscular activity in the stomach. The doctor passes a thin tube down the patient’s throat into the stomach. This tube contains a wire that takes measurements of the electrical and muscular activity of the stomach as it digests foods and liquids. This helps show how the stomach is working, and if there is any delay in digestion.
- Esophagogastroduodenoscopy (also called EGD or upper endoscopy). This is a procedure that allows the doctor to examine the inside of the esophagus, stomach, and duodenum. A thin, flexible, lighted tube, called an endoscope, is guided into the mouth and throat, then into the esophagus, stomach, and duodenum. The endoscope allows the doctor to view the inside of this area of the body, as well as to allow instruments through the scope for the removal of a sample of tissue for biopsy (if necessary). Sedation is required for this test. Learn more about endoscopy.
What is the treatment for gastroparesis?
Our pediatric gastroenterologists and dietitians work with patients, their family and referring physicians and other medical specialists to develop a treatment plan that is mindful of each patients overall health, social and emotional needs. Specific treatment for gastroparesis will be determined based on:
- The child’s age, overall health and medical history
- Extent of the condition
- The child’s tolerance of specific medicines, procedures or therapies
- Expectations for the course of the condition
- The family’s opinion or preference.
Gastroparesis is usually a chronic condition, so treatment does not cure the condition, but rather helps the patient manage the condition. In gastroparesis related to diabetes, the primary goal is to regain control of the blood glucose levels.
Treatment may include:
- Medications. Several medications are used to treat gastroparesis. The child’s physician may prescribe combinations of medications or different medications to determine which is the most effective. Botulinum toxin (Botox) has also been shown to improve symptoms when injected directly into the pyloric sphincter.
- Dietary modifications. Changing eating habits can also help control gastroparesis. Sometimes, eating six smaller meals a day is more effective than eating three larger ones. Some doctors recommend several liquid meals a day until blood glucose levels are stable and gastroparesis is stable. The child’s doctor may also recommend avoiding fatty and high-fiber foods, as these can slow digestion and be difficult to digest. It is important to consult the child’s doctor or dietitian for the best eating plan for their condition.
- Surgery. Occasionally, when other approaches fail, it is necessary to perform a surgical procedure called jejunostomy, in which a feeding tube is inserted through the skin on the abdomen into the small intestine. This tube then allows nutrients to be put directly into the small intestine, bypassing the stomach. This is used only when gastroparesis is severe and prevents the nutrients and medications necessary to regulate blood glucose levels from reaching the bloodstream.A new surgically implanted device, known as a “gastric neurotransmitter,” may also be used to control nausea and vomiting.
- Parenteral nutrition. An alternative to the jejunostomy tube is parenteral nutrition (TPN), in which nutrients are delivered directly into the bloodstream, bypassing the digestive system. The doctor places a catheter in a chest vein, leaving an opening on the outside of the skin. A bag with liquid nutrients or medication can be attached to the catheter, allowing the fluid to enter the bloodstream through the vein. Learn more about TPN.












