Specialized Care for Children and Teens

When a child is ill and needs hospitalization, we understand that the entire family is affected. CHOC strongly believes in allowing a child to be a child and creating a sense of normalcy through play, discovery and creativity. That’s why we are dedicated to offering the most comprehensive support programs in the region, so kids don’t have to give up being kids. The Cancer Institute offers patients and families:
- One-of-a-kind hospital experience with child life services, activities, special events and much more.
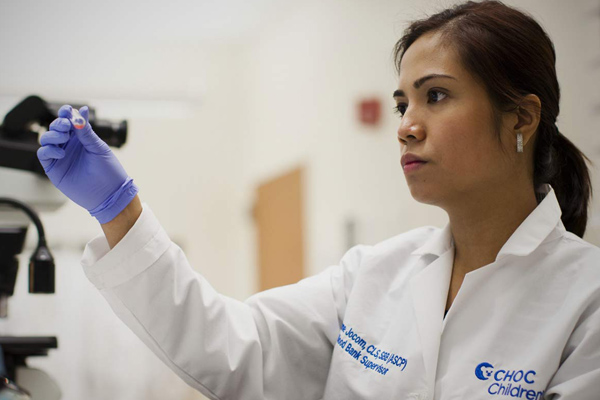
- Comprehensive diagnostic services.
- Outstanding outpatient services, including a dedicated clinic, outpatient infusion center and radiation therapy center.
- Pediatric cancer second opinions to provide reassurance when making decisions about your child’s care.